therapy
What is Cognitive Behavioral Therapy?

Cognitive Behavioral Therapy (CBT) stands as one of the most extensively researched and effective forms of psychotherapy in modern mental healthcare. With over 2,000 clinical trials supporting its efficacy, CBT has revolutionized how we understand and treat mental health conditions.
What is Cognitive Behavioral Therapy?
Cognitive Behavioral Therapy is a structured, evidence-based psychotherapy that focuses on the interconnected relationship between thoughts, emotions, and behaviors. Unlike traditional psychoanalytic approaches that delve deep into past experiences, CBT emphasizes current problems and practical solutions.
The core principle of CBT is elegantly simple yet profoundly effective: our thoughts influence our emotions, which in turn affect our behaviors, creating a cycle that can either support or undermine our mental wellbeing. By identifying and modifying negative thought patterns and maladaptive behaviors, individuals can break free from cycles of distress and develop healthier coping strategies.
How CBT Works
CBT operates through several key mechanisms that make it uniquely effective. The therapy is typically structured, goal-oriented, and time-limited, usually lasting between 12-20 sessions. Therapists and clients work collaboratively to:
- Identify automatic negative thoughts and cognitive distortions
- Examine the evidence for and against these thoughts
- Develop more balanced, realistic thinking patterns
- Practice new behaviors that support positive change
- Build practical coping skills for real-world situations
The therapy employs specific techniques such as cognitive restructuring, behavioral activation, exposure therapy, and mindfulness practices. Each technique is tailored to address specific symptoms and individual needs.
To illustrate how CBT works in practice, consider Sarah, a 28-year-old marketing professional who began experiencing panic attacks before important presentations. Her story demonstrates the CBT process in action.
Sarah's automatic thoughts were: "I'm going to embarrass myself," "Everyone will see I'm incompetent," and "My career is ruined if this goes badly." These catastrophic thoughts triggered intense anxiety, racing heart, and sweating. Her behavior became avoidance, she started calling in sick on presentation days, which only reinforced her fears.
Through CBT, Sarah learned to identify these automatic thoughts and examine the evidence. Her therapist helped her realize that in five years of presenting, she had never actually embarrassed herself significantly, and colleagues often praised her work. She practiced more balanced thoughts: "I'm well-prepared," "Some nervousness is normal," and "I can handle whatever happens."
Behaviorally, Sarah gradually exposed herself to presentation situations, starting with small team meetings and building up to larger groups. She learned breathing techniques and practiced relaxation exercises. Within three months, Sarah was presenting confidently again, having broken the cycle of catastrophic thinking that had trapped her in avoidance.
This example illustrates CBT's core principle: by changing how we think about situations and gradually changing our behaviors, we can transform our emotional responses and break free from cycles of distress.
The Evidence: CBT Statistics and Research Findings
The effectiveness of CBT is supported by an unprecedented volume of research. A comprehensive meta-analysis of 409 trials involving 52,702 patients, the largest meta-analysis ever conducted for a specific type of psychotherapy, provides robust evidence for CBT's efficacy across multiple mental health conditions.
Key Effectiveness Statistics
- Response Rate: CBT demonstrates a 42% response rate across various mental health conditions
- Depression Treatment: Medium to large effect sizes (d = 0.75-0.95) in naturalistic settings
- Anxiety Disorders: CBT shows superior effects compared to waitlist controls, with significant improvements maintained at follow-up
- Long-term Effectiveness: Studies show CBT benefits are largely maintained over time, with only slight decreases at longer follow-up periods
- Youth Treatment: A study of 210 children with anxiety disorders showed stable long-term effects over 4+ years
Recent research from 2024 involving 6,624 patients across 29 university outpatient clinics found that only 1.9% of patients reported symptom worsening during CBT treatment, while 3.4% reported no change. The remaining 94.7% experienced some level of improvement.
Professional Perspectives: What Therapists Say About CBT
Mental health professionals consistently recognize CBT's unique strengths and practical applications. Their insights provide valuable perspective on why CBT has become the gold standard in psychological treatment.
"CBT is effective in treating depression, anxiety, post-traumatic stress disorder, eating disorders, personality disorders, anger problems, and general stress. The way we think determines the way we feel. This is a basic principle of cognitive behaviour therapy, a psychological approach widely used by mental-health practitioners all over the world."
CBT in the Digital Age: AI-Powered Mental Healthcare
The integration of artificial intelligence with CBT principles represents one of the most significant developments in modern mental healthcare. As traditional therapy faces challenges of accessibility, cost, and availability, AI-powered CBT interventions are emerging as a scalable solution to meet growing mental health needs.
The Current Landscape of AI Therapy
The AI mental health market has experienced explosive growth, with projections showing expansion from $1.13 billion in 2023 to $5.08 billion by 2030, a compound annual growth rate of 24.10%. This growth reflects both technological advancement and urgent healthcare needs, as approximately 970 million people worldwide live with mental health disorders.
A recent survey revealed a striking trend: 48.7% of respondents using AI who reported mental health challenges are utilizing large language models like ChatGPT for therapeutic support. With 96% specifically using ChatGPT, this application may represent the single largest venue for mental health support in the United States, potentially serving more people than traditional institutional providers.
User data reveals interesting patterns in AI therapy adoption. The most common conditions for which people seek AI support are anxiety (79.8%), depression (72.4%), and stress (70%). Relationship issues, low self-esteem, and trauma also represent significant use cases.
Perhaps most remarkably, among users who have experience with both AI and human therapy, close to 75% reported their AI experience was on par with or better than human therapy. This suggests that AI interventions are not merely convenient alternatives but genuinely effective therapeutic tools.
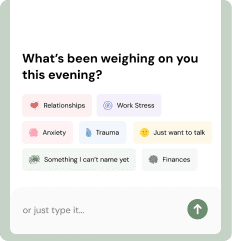
Renée: Pioneering the Future of AI Therapy
As the field of AI therapy continues to evolve, innovative platforms like Renée are demonstrating how CBT principles can be effectively integrated into AI-powered emotional support systems. Launched in July 2025, Renée represents a new generation of AI companions that go beyond simple chatbot interactions to provide meaningful emotional support.
Renée's approach reflects many CBT principles while adapting them for AI delivery. The platform focuses on helping users identify and process their emotions, challenge negative thought patterns, and develop healthier coping strategies, all core components of traditional CBT.
As research continues to validate AI therapy approaches and platforms like Renée refine their methodologies, we're witnessing the emergence of a new paradigm in mental healthcare, one that combines the proven principles of CBT with the accessibility and scalability of artificial intelligence.
You don't have to face this alone
Meet Renée, your consistent companion who's always here when you need someone to talk to, in your way text or call her. She remembers what matters to you, so you never feel like a stranger.
Talk to RenéeThe Future of CBT: Integration and Innovation
Cognitive Behavioral Therapy's journey from a revolutionary challenge to psychoanalytic orthodoxy to the most researched and widely practiced form of psychotherapy represents one of psychology's greatest success stories. With over 2,000 clinical trials supporting its effectiveness and applications spanning from depression and anxiety to chronic pain and substance abuse, CBT has proven its versatility and durability.
As we move forward, the integration of AI technology with CBT principles promises to address one of mental healthcare's greatest challenges: accessibility. While traditional therapy remains invaluable for complex cases, AI-powered interventions can provide immediate, affordable support to millions who might otherwise go without treatment.
The future of mental healthcare likely lies not in choosing between human and artificial intelligence, but in thoughtfully combining both approaches. CBT's evidence-based framework provides the perfect foundation for this integration, offering validated techniques that can be adapted for digital delivery while maintaining therapeutic effectiveness.
As platforms like Renée continue to innovate and researchers develop more sophisticated AI therapy approaches, we stand at the threshold of a new era in mental healthcare, one where the proven principles of CBT can reach anyone, anywhere, at any time. The therapeutic revolution that Aaron Beck started in the 1960s continues to evolve, promising hope and healing for generations to come.


